On the Forefront of Veterinary Medicine
Neuroscientists explore stem cell technology to understand what happens inside the dog’s brain after a seizure.
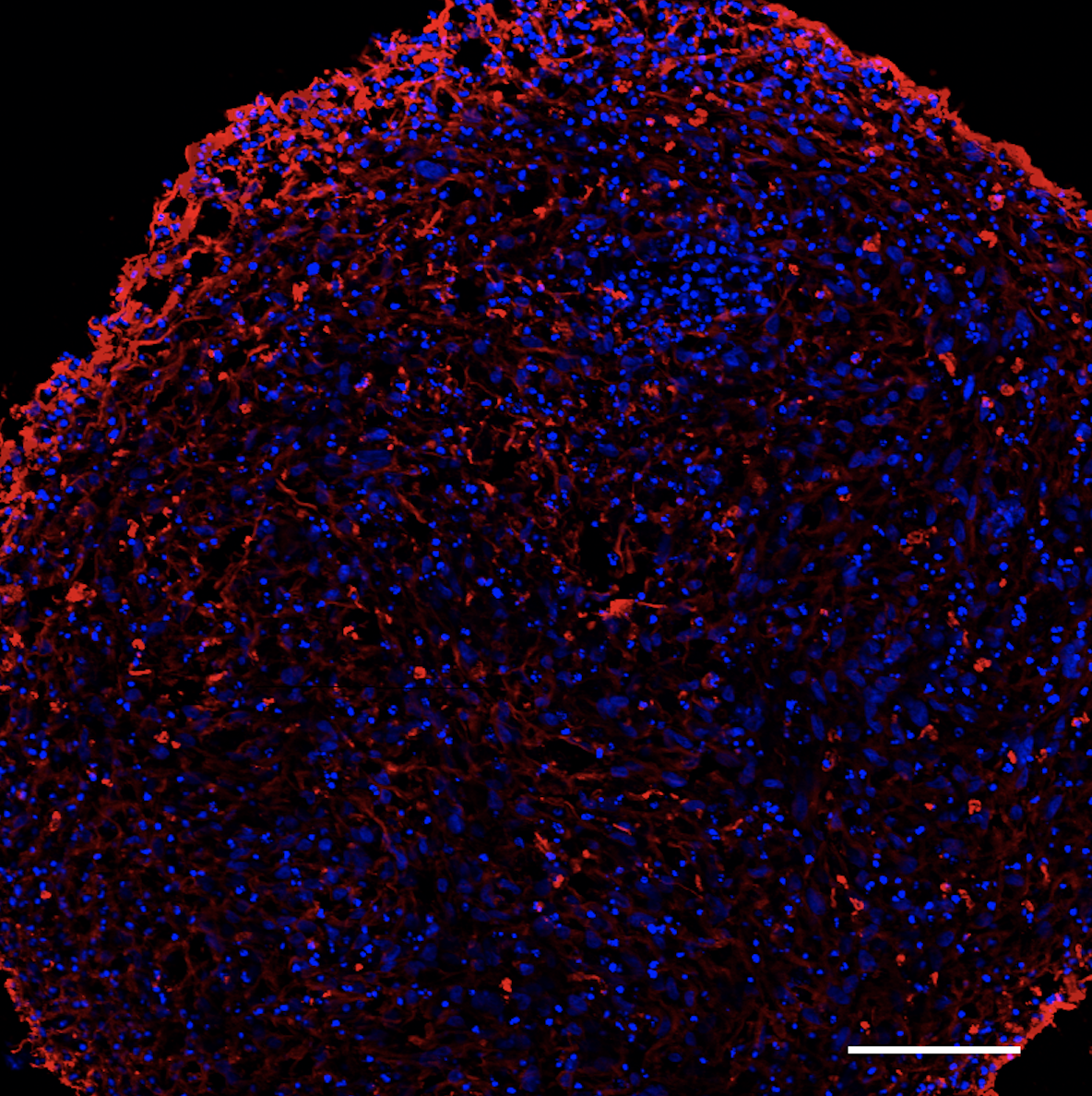
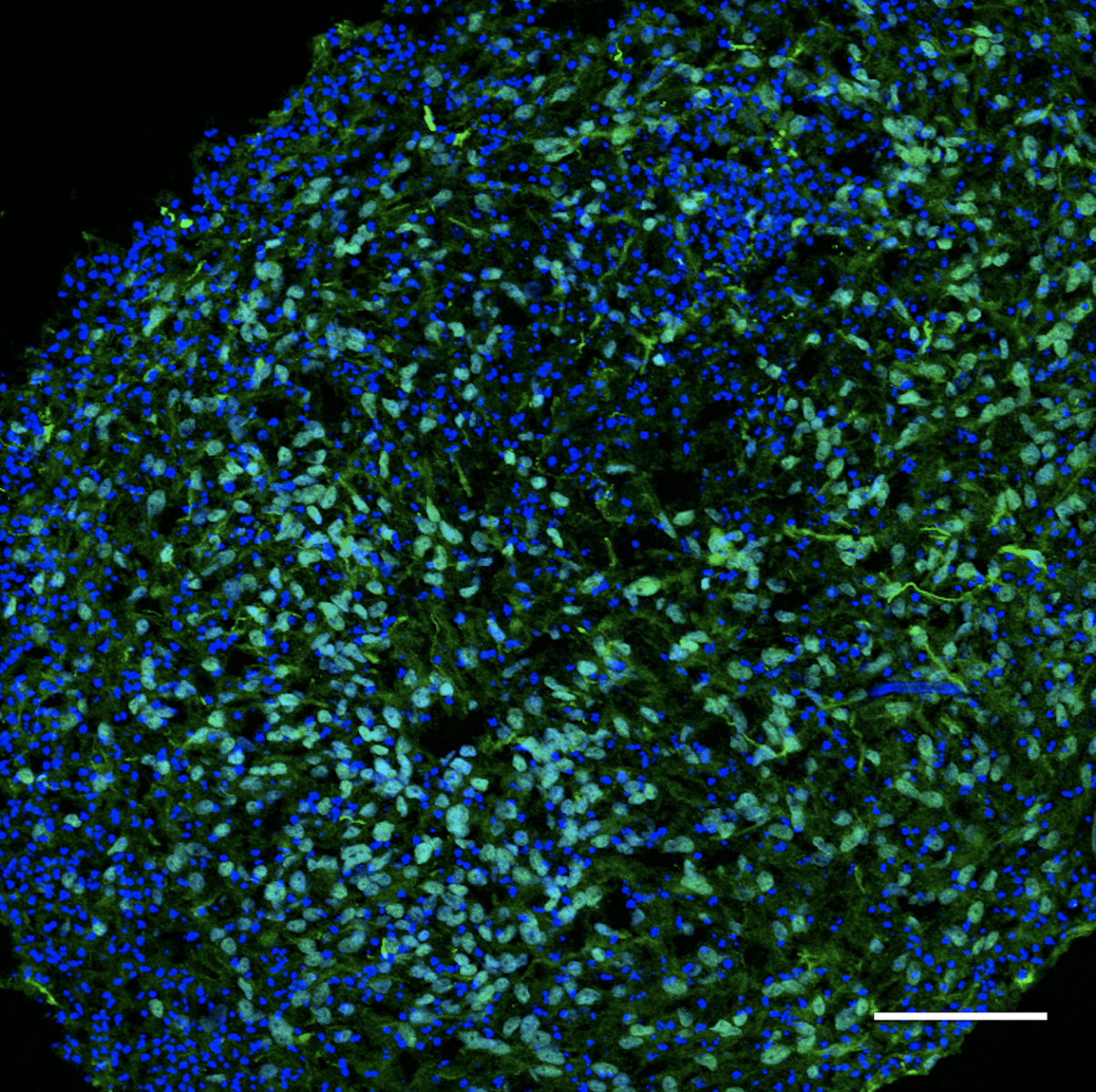
.png) A research team based at the University of Guelph’s (U of G) Ontario Veterinary College (OVC) is developing a cerebral organoid to address what happens inside a neuron in the brain after a dog has a seizure. A cerebral organoid is an in vitro miniature brain grown from stem cells; the organoid will serve as a 3-D model of a dog’s brain for the team to study neurological function, disease progression and behaviour patterns as well as possible treatments for epilepsy.
A research team based at the University of Guelph’s (U of G) Ontario Veterinary College (OVC) is developing a cerebral organoid to address what happens inside a neuron in the brain after a dog has a seizure. A cerebral organoid is an in vitro miniature brain grown from stem cells; the organoid will serve as a 3-D model of a dog’s brain for the team to study neurological function, disease progression and behaviour patterns as well as possible treatments for epilepsy.
Epilepsy is the most common neurological disorder seen in dogs and the most common type of brain condition in dogs and cats who are referred to the OVC Companion Animal Hospital.
Neurons are the fundamental unit of the brain responsible for processing and transmitting information throughout the nervous system. If signaling between cells is disrupted or if too many signals are sent at once, this may cause a seizure.
Idiopathic epilepsy is defined as recurrent seizures with no identifiable structural cause such as brain tumours, trauma, inflammation or biochemical cause such as low blood sugar or toxicity. Dogs with this type of epilepsy are typically diagnosed between six months and six years of age.
Dr. Thomas Parmentier, a board-certified veterinary neurologist and PhD candidate in the Department of Biomedical Sciences, is conducting this research along with advisors Drs. Jonathan LaMarre and Fiona James.
“The current treatment we have available to our veterinary patients with epilepsy involves prescribed medication to help manage and decrease the frequency of seizures but unfortunately, over time, many pets grow resistant to that treatment,” Parmentier explains, adding that up to one in three dogs with epilepsy will need two or more drugs to control their seizure frequency. These drugs can come with significant side effects.
“The burden that is caused with an epilepsy diagnosis on patients and their caretakers is very significant,” says Parmentier. “Identifying new treatment possibilities will have an important impact on the quality of life of pets impacted by the condition as well as their owners.”
The research team is specifically interested in what happens inside a neuron after a seizure occurs and how these changes, particularly in certain gene expressions (the process by which the instructions in DNA are converted into a functional product, such as a protein), contribute to the increase in seizure frequency and drug resistance. The collaborative team of clinicians and scientists hope their work will lead to the discovery of new therapeutic options for dogs that will both decrease seizure frequency and stop epilepsy progression altogether.
“We are investigating several mechanisms of regulation of gene expression that are impaired in neurons during a seizure,” explains Parmentier.
 One of those mechanisms is microRNA, small pieces of RNA, or ribonucleic acid, that regulate the expression of certain genes and how much of a particular protein is produced. Parmentier says these microRNA can serve both as biomarkers for specific conditions but also can be used as drugs to restore normal gene expression.
One of those mechanisms is microRNA, small pieces of RNA, or ribonucleic acid, that regulate the expression of certain genes and how much of a particular protein is produced. Parmentier says these microRNA can serve both as biomarkers for specific conditions but also can be used as drugs to restore normal gene expression.
“In other words, microRNA could help us predict if a particular case of canine epilepsy will be difficult to medically manage or not. It may also one day be given as a treatment for epilepsy itself.”
The research team also includes collaboration with investigators studying human brain function: Dean Betts at the Schulich School of Medicine and Dentistry at Western University and colleagues from U of G, Craig Bailey and Jasmin Lalonde.
“This technology, called ‘cerebral organoids’, is very new and as far as we know, has never been used for pets. This is a very exciting project because it allows us to safely grow a small piece of brain from stem cells in the lab and study how it responds to different treatments,” says LaMarre.
Once the “mini brain” is at the desired size, only a few millimeters, the goal is to stimulate the organoid to experience seizures, similar to what happens in the brain of epileptic dogs.
“The potential of this technology is huge as we will be able to track how neurons respond to seizures and test the effectiveness of new drugs,” says Parmentier, adding, that the ability to develop these organoids will provide a very valuable and non-invasive tool to understand a dog’s brain function and how it reacts to diseases.
While this research is still in its infancy the team hopes next steps will include a more personalized approach to medical cases, developing organoids directly from patients themselves by harvesting a small, minimally-invasive skin sample. The cells would then be reprogrammed in the laboratory into stem cells, a technology called induced pluripotent stem cells.
Parmentier adds, “the ability to study organoids created from epileptic patients will pave the way for more tailored therapies, or precision medicine, so that clinicians can prescribe the treatment plans that are most likely to help their patients based on genetic understanding of the disease.”
In photos: Mini brain under the microscope. Photo credit: Dr. Thomas Parmentier, LaMarre laboratory, Ontario Veterinary College, University of Guelph.
Read more in the fall / winter issue of Best Friends Magazine.